Some of the links in this post are affiliate links. We may earn an affiliate commission if you click on a link and purchase an item we recommend. This doesn’t add any additional cost to you, but helps support our business.
Top 7 Ways to Treat Plantar Fasciitis at Home
Plantar Fasciitis can be a frustrating condition to treat. It can take weeks, months, or even years to fully resolve. Our sports injury clinic in Mission Valley, San Diego specializes in treating chronic injuries, plantar fasciitis included. Check out our other blog post on how we treat plantar fasciitis in our office Plantar Fasciitis: Resolving Foot Pain with Active Release Technique (ART) and Graston. Along with treatment, here are the top 7 ways to treat plantar fasciitis at home.
Trigger Point Release Ball
Using a trigger point release ball and roller to help massage tight muscles of the foot and calf can help ease the symptoms of plantar fasciitis. We recommend the TriggerPoint Foundation Starter Kit  for self massage of the lower legs and feet. It has a durable and firm roller to address the calves and trigger point balls to use on specific points of the calves and bottom of the feet. Using them daily will help improve the quality of the tissues and help treat plantar fasciitis at home.
for self massage of the lower legs and feet. It has a durable and firm roller to address the calves and trigger point balls to use on specific points of the calves and bottom of the feet. Using them daily will help improve the quality of the tissues and help treat plantar fasciitis at home.
Calf Stretcher
If you have tight calves, and many of us do, daily stretching of the lower leg will help improve function of the foot and ankle. We recommend a dedicated Calf Stretcher & Foot Rocker  it allows for a really good stretch to the lower leg and foot. Using it to stretch multiple times throughout the day will help keep the muscles and tendons loose.
it allows for a really good stretch to the lower leg and foot. Using it to stretch multiple times throughout the day will help keep the muscles and tendons loose.
YogaToes
Stretching the toes out where the muscles, tendons, and fascia insert can help ease the symptoms of plantar fasciitis. We like YogaToes because they are thick, strong, and durable. Other devices we have found to break easy, or do not offer a good enough stretch in most cases. Where YogaToes when sitting at home, move your toes in a stretched position. They can be very valuable to treat plantar fasciitis at home especially if you have other signs of toe deformity such as bunions.
because they are thick, strong, and durable. Other devices we have found to break easy, or do not offer a good enough stretch in most cases. Where YogaToes when sitting at home, move your toes in a stretched position. They can be very valuable to treat plantar fasciitis at home especially if you have other signs of toe deformity such as bunions.
Heel Cups
One of the ways to ease the symptoms of plantar fasciitis is to stay off of your feet when it hurts. For most people, that is nearly impossible! Tuli’s Heavy Duty Gel Heel Cups are designed to placed in you shoes and absorb shock transmitted to the heel from walking and standing. We also like heel cups as they squeeze your heel together from the sides. This reinforces the heels fat pad to help bolster your natural heel cushion.
are designed to placed in you shoes and absorb shock transmitted to the heel from walking and standing. We also like heel cups as they squeeze your heel together from the sides. This reinforces the heels fat pad to help bolster your natural heel cushion.
Night Splint
Classic plantar Fasciitis symptoms include sharp, dagger like pain in the bottom of the heel. These symptoms are worse during the first steps out of bed in the morning. This is due to the tissues tightening up over night and then getting rapidly/forcefully stretched when you stand up and put weight on the plantar fascia. A Plantar Fasciitis Night Splint helps keep the fascia and lower leg muscles in a stretched position over night to reduce the pain in the morning. It can be highly effective to treat plantar fasciitis at home.
helps keep the fascia and lower leg muscles in a stretched position over night to reduce the pain in the morning. It can be highly effective to treat plantar fasciitis at home.
The one complaint we hear from patients is that it is difficult to sleep through the night with it on as it is bulky and awkward. If sleeping is a challenge, then where the brace when you are stationary for extended periods of time to maintain flexibility to the fascia. The next item on the list is a similar device but tends to offer a bit more comfort for sleeping.
Strassburg Sock
The Strassburg Sock is another device to be used when sleeping to help maintain flexibility to the foot and lower leg muscles. One reason we like it better than a splint is that it pulls the toes back to get a better stretch. The two complaints we hear are difficult to sleep with and the sock can compress the calf too much. If sleeping with the sock is too difficult, wear it when you are stationary for long periods of time.
is another device to be used when sleeping to help maintain flexibility to the foot and lower leg muscles. One reason we like it better than a splint is that it pulls the toes back to get a better stretch. The two complaints we hear are difficult to sleep with and the sock can compress the calf too much. If sleeping with the sock is too difficult, wear it when you are stationary for long periods of time.
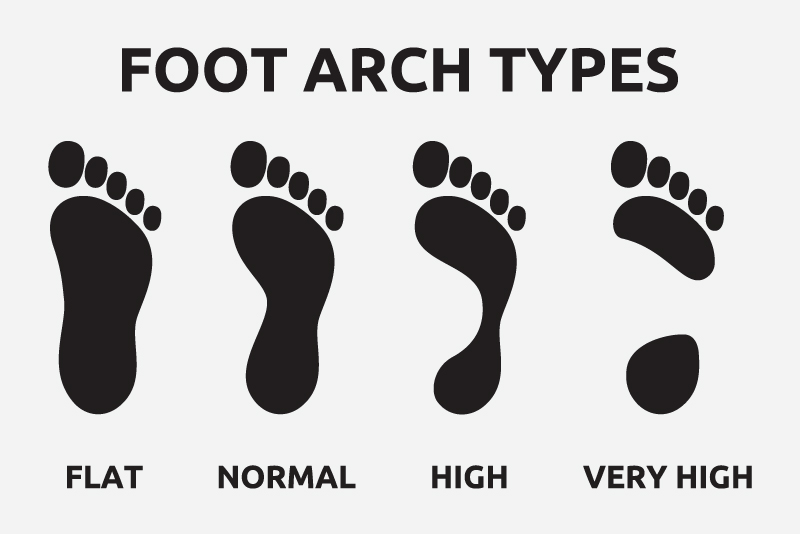
Arch Support
The final recommendation is arch support to help support the plantar fascia. In cases of low arches, extra support to the arch and heel can help ease the symptoms of plantar fasciitis. We recommend Superfeet GREEN Full Length Insole for a couple of reasons. If the goal is arch support, you need something firm enough to actually support the arch. Too many insoles are too soft and do not offer any support whatsoever. Superfeet insoles are made form hard plastic or carbon (depending on models). They support the arch sufficiently. Another reason we prefer Superfeet, is that they have deep heel cups in the insole. This can help bolster the padding around the heel to offer symptom relief.
for a couple of reasons. If the goal is arch support, you need something firm enough to actually support the arch. Too many insoles are too soft and do not offer any support whatsoever. Superfeet insoles are made form hard plastic or carbon (depending on models). They support the arch sufficiently. Another reason we prefer Superfeet, is that they have deep heel cups in the insole. This can help bolster the padding around the heel to offer symptom relief.
These are the top 7 ways to treat plantar fasciitis at home. Please keep in mind that these are general recommendations. We always recommend getting a proper evaluation by a health care provider. If you are in San Diego, our injury treatment clinic is conveniently located in Mission Valley. We are located near Hillcrest, Normal Heights, University Heights, North Park, South Park, and Downtown. Our Sports Chiropractors are trained to diagnose, manage, and treat plantar fasciitis. We also offer Acupuncture, Personal Training, and Massage. Please schedule using our online scheduling application or call our office at 619-818-4306 today!