Sports injuries are injuries that occur in athletic activities. They can result from acute trauma, or from overuse of a particular body part
The Hidden Cost of Resting Your Injury
/in running injury, Shockwave Therapy, Shockwave treatment, Sports Injury, Training/by adminStruggling with deep, nagging pain in your lower glute that flares up when you sit or run? Upper hamstring tendinopathy can be stubborn, but a combination of shockwave therapy and progressive exercise rehab is the key to lasting relief and tendon resilience—learn why this approach works best!
Upper Hamstring Tendinopathy: Why Combining Shockwave Therapy with Exercise Rehab Is a Game Changer
/in running injury, Shockwave Therapy, Shockwave treatment, Sports Injury, Training/by adminStruggling with deep, nagging pain in your lower glute that flares up when you sit or run? Upper hamstring tendinopathy can be stubborn, but a combination of shockwave therapy and progressive exercise rehab is the key to lasting relief and tendon resilience—learn why this approach works best!
Is Running BAD for your discs?
/in Low Back Pain, Low back Sports Injury, running injury, Uncategorized/by adminRunning and Your Spine: A New Look at Intervertebral Disc Health
There’s a common myth that running is bad for your back. But a new systematic review published in Sports Health tells a different story. This review combined 13 studies with 632 participants to investigate how running affects the health of intervertebral discs—the cushions between the vertebrae in your spine.
How Running Affects Your Spine
The review looked at two types of studies: some measured how running affected spinal height, while others used MRI to observe changes in disc composition. Here’s what the research found:
- Temporary Compression: Running causes temporary compression of the discs. This means that during a run, discs lose some water content and slightly shrink in height.
- Supercompensation Between Runs: After the run, your discs supercompensate by drawing water and glycosaminoglycans back in. These are important for keeping your discs hydrated and healthy. Over time, this process can actually improve disc health.
- Stronger, Healthier Discs: Habitual runners were found to have healthier and stronger discs than non-runners. So rather than damaging your spine, regular running appears to build resilience in your intervertebral discs.
Takeaways for Runners
This study is great news for runners and those hesitant to start due to back pain concerns. Here’s what you should know:
- Running is Safe for Your Back: The temporary disc compression during a run is completely normal and healthy. The key is the recovery between runs, where your body replenishes lost fluids and nutrients.
- Regular Running Builds Stronger Discs: Over time, the cycles of compression and supercompensation make your discs more resilient, reducing the risk of spinal issues.
- No Need to Fear Running: If you’ve been avoiding running due to fears of back injury, this study shows that running is not only safe but can actively improve your spinal health.
Incorporating regular runs into your routine can be a powerful way to maintain a healthy back. So, lace up those running shoes and start reaping the benefits for your spine!
Reference: Shu D, Dai S, Wang J, Meng F, Zhang C, Zhao Z. Impact of Running Exercise on Intervertebral Disc: A Systematic Review. Sports Health. 2024;0(0). doi:10.1177/19417381231221125
Types of Heel Pain
/in Foot pain, running injury, Sports Injury/by Dr. Travis RoseMany patients ask themselves, “Do I have plantar fasciitis?”. Many patients assume they have plantar fasciitis as it is a fairly well known term but there are many types of heel pain. The types of heel pain shown in the video below are the most common types of heel pain. Based on the location and the type of pain you are experiencing, it is easy to differentiate between let’s say plantar fasciitis or achilles tendonitis, plantar fasciitis or fat pad syndrome, etc. Once you have a proper diagnosis, then you can go about treatment for heel pain successfully.
What is Fat Pad Syndrome?
The most common condition we see that tricks patients into thinking they have plantar fasciitis is fat pad syndrome. Some patients can have both! There are a few key differences in the history and exam to differentiate between the two. Patients with fat pad syndrome have pain consistently throughout the day, worse barefoot, and stretching does not help. Plantar fasciitis is characterized by pain that is worse in the morning, but improves to a degree as you walk around. Stretching and rolling usually help temporarily alleviate symptoms. Fat pad syndrome needs to be protected with taping to support the fat pad, wearing heel cups in your shoes, and wearing cushioned shoes throughout the day. Once the heel is protected, inflammation will go away and the symptoms improve.

Is a Plantar Heel Spur the Cause of My Pain?
One question we often get asked is if a patient has plantar fasciitis or heel spur. The reality is, is that people may have heel spurs and never have pain in the heel. Or patients may have plantar fasciitis symptoms and find a bone spur after having an x-ray. Patients may experience plantar fasciitis pain with a heel spur or they may not.
A heel spur is only present if there has been enough tension or pulling from the plantar fascia. This constant tension results in the heel bone becoming elongated at the plantar fascia attachment site. This usually occurs from long standing tension in the plantar fascia from high arches, biomechanical stress, hallux limitus, etc. Treatment is same if a patient has plantar fasciitis or heel spur.
Achilles Spurs and Haglund’s Deformity
Heel spurs can also be seen on the back side of the heel where the Achilles tendon attaches. Achilles tendonitis can cause pain in the back of the heel. This type or Achilles tendinopathy is termed insertional Achilles tendonitis as the pain is at the site of where the tendon inserts into the heel bone. Similar to the plantar heel spur, some patients may have an Achilles heel spur, others may not. Treatment of insertional Achilles tendinitis, with or without a spur is the same.
A more obvious deformity called a Haglund’s deformity, is a overgrowth on the backside of the heel where the Achilles attaches. The tendon becomes inflamed when this deformity rubs on the soft tissues, especially in shoes. We most comonly see this in patients who have had chronic Achilles tendinopathy or have other structural causes of this deformity such as high arches, hallus limitus, and or rear foot varus
Less Common Types of Heel Pain
L
Less common types of heel pain but still seen in the clinic are peroneal tendonitis and posterior tibialis tendonitis. Peroneal tendonitis can affect the outer portion of the heel while posterior tibialis tendonitis can affect the inner heel area. Usually the pain is at the sides of the heels but we have seen some cases where pain is on the bottom/side of the heel. Again patients are quick to say they have plantar fasciitis, but with a pinpoint exam, we can rule in these other tendons as being the pain generators, not the plantar fascia.
The heel is a small area and can be relatively simple to diagnose the cause(s) of heel pain. However, many people end up having different conditions than what they thought they had. This ultimately delays the recovery process by not receiving the correct treatment plan initially. Schedule with one of our sports chiropractors today to get you on the correct path to recovery. Peak Form Health Center is located in Mission Valley, San Diego.
Achilles Tendinitis Exercises
/in Achilles Tendinopathy, Sports Injury/by Dr. Travis RoseWe demonstrate Achilles Tendinitis exercises in the video below. Achilles tendinitis exercises that focus on loading the Achilles tendon have been shown to have significant outcomes in pain and function. Many Achilles tendonitis rehab plans fall short by showing patients very low level exercises such as stretches and foam rolling. That is not to say those exercises are not helpful for a patient, they might be. With a successful achilles tendinopathy exercise program, we have find the most challenging strength exercises that patients do well. If a patient has been performing the same exercises for 12 weeks, they are not being challenged sufficiently!
Every achilles tendinopathy rehab program is different. A patient may start achilles tendon exercises at a different point than the next. It depends on the patient’s achilles tendonitis exercise tolerance to Achilles tendon loading and goals around the outcome of treatments. A sedentary individual with a goal of walking pain free will have a significantly different program from an in season college basketball player.
Example of Achilles Tendinitis Exercises

A recent patient dealing with Achilles tendinitis is a high level amateur tennis player and plays pickleball for fun. She had Achilles tendinitis for 1 month, with prior history of multiple calf strains on that leg. She did not seek treatment as she thought the pain would subside. The pain slowly worsened until she was unable to play tennis and pickleball due to Achilles Pain.
Achilles Tendinitis Exam and Treatment
We went through a thorough Achilles tendinitis exam and treatment on the first visit. The lower leg with achilles tendinitis was significantly more weak than the other leg. For example, we performed a single leg calf raise endurance test. The uninjured leg, she performed 40 easily in 1 minute. On the injured side, she performed 20, with poor movement quality starting at 8! An important note, she felt some soreness but it did not get worse with challenging the tendon with exercise.
Challenge with Exercise
Knowing pain was not a limiting factor, we were able to prescribe daily, calf loading exercises to improve strength. This was the obvious improvement that was needed to help her injury. After 2 weeks, she showed significant improvement in pain. She was able to perform the same number of reps unbroken as the healthy leg at that point. At this point we progressed to dynamic exercises such as pogo hops, squat jumps, and four square hops. She had minor discomfort at first, but as she performed the plyometrics pain started to dissipate and confidence increased.
It was very important to keep progressing this tennis athlete quickly, and get her to more sport specific activities. This, with graduated return to play, will help avoid recurrence of Achilles injury, and avoid future injury.
If you are looking for a well rounded assessment and detailed treatment plan, schedule with us! Don’t let prior poor physical therapy for Achilles tendinitis deter you from finding the right treatment approach. Our team of sport chiropractors are trained to assess, treat, and prescribed exercises for achilles tendinitis and other causes of heel pain. We are located in Mission Valley, San Diego near the neighborhoods of La Jolla, Scripps Ranch, and Point Loma!
Achilles Tendinitis Treatment
/in Achilles Tendinopathy, Shockwave Therapy, Sports Injury/by Dr. Travis RoseWhat is Achilles Tendinitis and Tendinopathy?
When looking for Achilles tendinitis treatment, it is first important to understand the condition. Achilles tendinitis is characterized by pain, and sometimes swelling along the Achilles tendon. Achilles tendinosis is pain that has become chronic (lasting 3+ months). At this stage of the injury, the tendon begins to show degenerative changes. Achilles tendinopathy is more of an umbrella term for pain and dysfunction at the Achilles tendon. Achilles tendinopathy is a product of applying load to the tendon which exceeds the ability of the tendon to withstand load.
For example, a completely sedentary individual decides they want to start walking daily. They begin walking 5 miles per day up steep hills. After 3 weeks, they develop Achilles tendinitis in both lower legs. Why? The tendons were not in good condition with minimal activity demands, and then were put in a position of high strain (5 miles walks). Couple that with very minimal recovery between sessions (performing every day) and Achilles tendinitis may develop. If that same individual began their exercise program walking every other day, on flat ground starting with 10 minutes and slowly increasing the time of the walks, they would have likely have much more success in properly introducing strain to the tendons to avoid injury!
Treatment Methods
Achilles tendinitis treatment generally consists of controlling the pain. Activity modification, NSAIDS, ice/heat, various manual therapy, and stretching to the calf muscles help with this aspect. In the video above, we discuss examination procedures for the Achilles and lower leg. We also show treatment options such as Active Release Technique for Achilles tendinitis, and Graston Technique for Achilles tendinitis. Active Release Technique involves identifying tight portions of the muscles that are causing excessive tension on the Achilles tendon. Once identified, the practitioner shortens the muscle, applies firm pressure and has the patient actively lengthen the muscle. This helps loosen the muscle, break down adhesions in the muscle fibers, and promotes blood flow for healing.
Graston technique for achilles tendinopathy involves using metal tools to rub along the Achilles tendon. This promotes blood flow to the the tendon which helps promote healing to the injured tendon. The manual treatments are designed to help decrease pain and allow the patient to strengthen the tendon successfully. For long term resolution of achilles tendinopathy, loading exercises are key.
Shockwave for Achilles Tendinitis
A new treatment modality has been shown to be effective at helping resolve chronic Achilles tendinopathy. Shockwave therapy utilizes high energy sounds waves which penetrate deep into the tissues. This results in improvement in blood flow, break down of scar tissue, and improve the healing response to the injured area. Read more about shockwave therapy here.

Exercises for Tendinopathy
The most recent literature in the past several years shows that Achilles tendinitis treatment must include loading exercises to the Achilles tendon. Various eccentric, isometric, concentric loading exercises have been tested and shown to help decrease symptoms while strengthening the tendon/muscle complex. When Achilles tendonitis exercises are performed, it is ok to work through some pain. As the function of the muscles and tendons improve, the pain will begin to dissipate and not return. Achilles exercises take patience, and consistency but will help significantly with Achilles tendinitis symptoms. Ultimately, strengthening, and proper return to play will help avoid nagging Achilles tendinitis symptoms. Check out our achilles tendinitis exercise video for examples of progressions we use in the office.

High Hamstring Tendinopathy Treatment
/in Knee Pain, running injury, Shockwave Therapy, Shockwave treatment, Sports Injury/by Dr. Travis RoseHigh hamstring tendinopathy is a condition that affects many different athletes. This type of injury is usually a result of repetitive strain, and affects many running athletes. Track running athletes, particularly hurdlers, are susceptible to high hamstring tendinopathy due to the large forceful range of motion required. Endurance runners are also susceptible due to the high volume of contractions the hamstring muscles undergo during training and racing. Usual treatment for high hamstring tendinopathy involve massage, Active Release Technique, Graston Technique, eccentric loading exercises (Nordic hamstring curls), and core strengthening.
Shockwave Therapy for High Hamstring Tendinopathy
In stubborn cases of high hamstring tendinopathy, we have been having great success with shockwave therapy. High hamstring tendinopathy treatment with shockwave therapy involves using shockwaves to stimulate a healing response at the affected hamstring tendon. Shockwave therapy has been shown to increase blood supply, activate dormant stem cells, break down trigger points, and loosen up scar tissue/calcifications at the injured site.
In chronic tendinopathy, the affected tendon has poor blood supply and physically starts deteriorating. The shockwaves stimulate the body’s healing response to the area to regenerate the damaged tendon. With weekly treatments, the beneficial inflammation/healing response reaches its peak to repair the damaged tissue.
Watch a shockwave treatment with one of our marathon runners who was dealing with nagging high hamstring tendinopathy.
After 4-8 weeks, most patients experience complete resolution of their high hamstring tendinopathy. Most importantly, patients do not need to avoid training while you are undergoing shockwave therapy treatments. In fact, it is important to load the hamstring with targeted strength exercises. Eccentric loading exercises such the Nordic hamstring curl are very effective at targeting the hamstrings. Even simple isometric exercises are enough to stimulate the tendon while it undergoes shockwave therapy. If you are interested in starting your shockwave therapy for high hamstring tendinopathy, schedule here. We also treat various other tendinopathies with shockwave therapy.
Golfer’s Elbow Treatment
/in Conditions, Elbow pain, Sports Injury/by Dr. Travis RoseWhat is Golfer’s Elbow
Golfer’s elbow or medial epicondylitis is characterized by pain at the inner portion of the elbow. It is considered a repetitive strain injury and develops when load exceeds the current resiliency of the muscles and tendon. The flexor muscles (the muscles that help you make a fist), as well as the pronator teres muscle (helps us turn a doorknob) all share the common flexor tendon. The common flexor tendon attaches to the upper arm bone at the medial epicondyle. Conversely, tennis elbow is characterized by pain on the outer portion of the elbow.
With repetitive stress to the forearm muscles, the tendon bone attachment initially becomes inflamed resulting in pain. If left undiagnosed, the tendon no longer is inflamed and actually starts degenerating and is termed tendinopathy. Most cases of Golfer’s elbow affect patients for a long time so the more appropriate term is medial epicondylopathy. Check out our video below for a demonstration on the exam and treatment for Golfer’s elbow.
Who is Susceptible to Golfer’s Elbow?
As the name suggests, golfer’s commonly are affected by this condition due to the nature/impact of the golf swing. Any profession or activity that uses the hands at a high level are also very susceptible. Mechanics, software engineers, office employees, body builders, powerlifters, rock climbers, swimmers etc. all place a high amounts of load into the forearm muscles and can lead to medial epicondylopathy. Again, development of Golfer’s elbow is usually due to prolonged low grade strain tasks like using a screwdriver. But can also be from a shorter but more forceful strain such as golf swings/weight lifting etc.
Treatment for Medial Epicondylitis
Treatment is multifactorial to help get rid of nagging Golfer’s elbow and conservative management offers lasting results. Graston technique and Active Release Technique are therapies that help ease the pain and loosen up tight restricted muscles that cause Golfer’s elbow. While these offer relief from pain, strengthening area will allow for further resiliency of those tissues. Check out our video, Flexbar Exercises for Golfer’s Elbow, to find a demonstration of a flexbar for Golfer’s Elbow. With ongoing loading of the the tendon, permanent results will occur and patients will be pain free.

If you are dealing with elbow pain, please schedule with one of our sports chiropractors today. Click the “schedule now” tab above or call our office at 619-818-4306. We are conveniently located in Mission Valley, San Diego. We will evaluate, diagnose your elbow pain and get you on a proper treatment plan to help you get rid of Golfer’s elbow.
Peroneal Tendonitis Treatment
/in Conditions, Foot pain, running injury, Sports Injury/by Dr. Travis RoseWhat is Peroneal Tendonitis?
Peroneal tendonitis is characterized by pain and tenderness on the outer part of the foot and ankle. In some cases, there can also be swelling around the tendons and tendon sheaths around the outer ankle. The two main peroneal muscles originate on the outer lower leg bone (fibula). The longer peroneal muscle runs around the outside of the ankle, and wraps around the side of the foot to the bottom of the foot and inserts into the midfoot (medial cuneiform) and the base of the 1st metatarsal. When these muscle become excessively tight, the tendons become inflamed, rub against the side of the ankle and foot which can become quite painful. Check out our video below describing our approach to treating peroneal tendonitis and continue reading below.
What are the Causes?
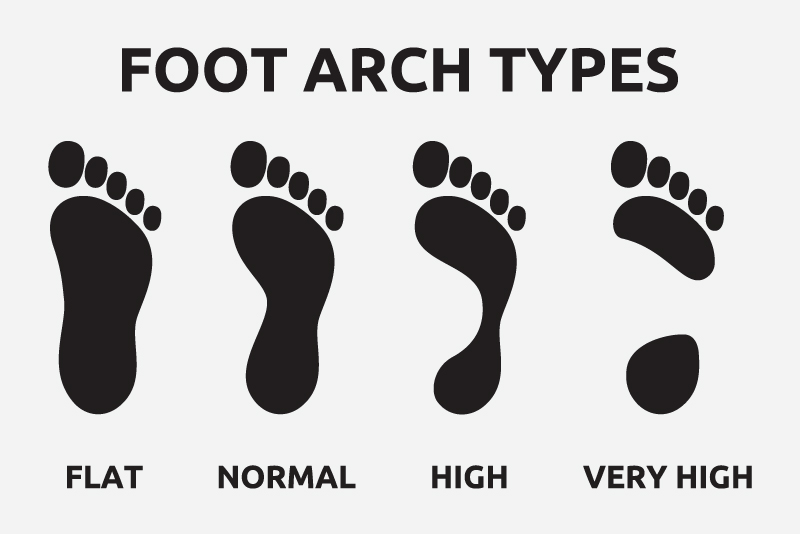
When the peroneal muscles sustain a higher load than what they are capable of handling, peroneal tendonitis can occur. Peroneal tendonitis can be a result of ankles sprains, repetitive strain (ballet dancing, jumping, running), people with high stiff arches in their feet, and from compensation due to other injuries (plantar fasciitis).
High stiff arches in the feet is often a presentation we see as this type of foot places more pressure on the outer half or outer third of the foot. This causes the peroneals to work much more strenuously than in feet with a more normal/flexible arches. Due to this weight distribution, these individuals are more prone to “rolling” their ankle during normal day to day walking and especially during sports (ex: Soccer). When looking at wear patterns on the bottom of shoes for a runner, we will see excessive where on the outer border of the bottom of the shoe. In many of the chronic cases of peroneal tendonitis, many patients do not know what “caused” the pain to start. When we go through a thorough exam and history, many patients have the history and characteristics described above which should be addressed for proper treatment.
Conservative Treatment
Conservative treatment for peroneal tendonitis and peroneal tendinopathy is very successful for managing the symptoms. In our office, we usually start peroneal tendonitis treatment with Graston Technique to the peroneal muscles (The peroneous longus, peroneous brevis, and peroneous tertius) to help loosen up the muscles while promoting blood flow to the area. Active release technique, a type of myofascial release, for peroneal tendonitis may be helpful to break down adhesions and trigger points within the peroneal muscles. Most importantly, loading the peroneal muscles with proper strength training exercises will help stimulate the injured areas of the tendon while providing strengthening to avoid future reaggravation. Peroneal tendonitis rehab exercises are crucial to help the tendons heal properly.
Finding the Root Cause of Peroneal Tendonitis
In treating peroneal tendonitis, it is important to discover the root cause. As described above, if a patient has very stiff, high arches, this will place more of the body weight on the outer half of the foot which will overly stimulate the peroneal muscles. Another example is peroneal tendonitis due to hallux limitus (when the big toe has limited extension), patients will have a hard time shifting their weight towards their big toe during gait which keeps their weight on the outer half of the foot, loading the peroneal muscles excessively.
Other conditions such as plantar fasciitis can lead to peroneal tendonitis due to compensation. When the bottom of the inner heel is painful, patients unknowingly keep the weight of their body on the outer half of the foot to avoid pressing into the painful part of the heel; peroneal muscles again become strained resulting in peroneal tendonitis. Many of these patients experience outer heel pain while walking or outer heel pain while running. Another condition called cuboid syndrome causes peroneal tendonitis as the peroneal tendons run across a portion of the cuboid bone. When the cuboid bone is stiff and not moving well with cuboid syndrome, the peroneal tendons also become stiff resulting in pain.
If you are dealing with peroneal tendinopathy, please schedule with one of our sports chiropractors today. Above you will find the “schedule now” tab which will direct you to our online scheduler. You may also call our office at 619-818-4306.
PEAK FORM NEWSLETTER SIGN UP
Our Office