Preventing Soccer Injuries
Soccer is an excellent way to build endurance, improve speed and stay in shape, all while enjoying being a part of a team. Nevertheless, soccer does involve quick start-and-stop motions and physical contact, which can lead to injury. The risk of injury is no reason not to play soccer however. Players simply need to be aware of the risks and know what steps they can take to play as safely as possible.
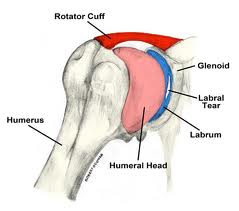
Sprains and strains are very common injuries in soccer, with varying forms of severity. Other injuries could include stress fractures and muscle strains from repeated overuse and direct blows to the body. Soccer players are also prone to shin splints, patellar tendinitis, and Achilles tendinitis. These injuries occur in the lower extremities, whereas neck sprains and concussions are common in the upper extremities. Injuries to the head, neck face are sometimes unavoidable. Just like wrist sprains, fractures and shoulder dislocations are unfortunately common due to falls and player-to-player contact.
The best place to start in prevention of these injuries is to have a pre-season physical examination and follow your doctor’s recommendations during the season. Using well-fitting cleats and shin guards is important in prevention. Molded and multi-studded cleats may be safer than screw-in cleats. Stay hydrated when out on the field and maintain proper fitness throughout the sport’s season. Injury rates are known to be higher in athletes who have not adequately prepared physically and remember to stretch adequately before and after your time on the field. After being inactive in the sport, progress gradually back to full-contact soccer through activities such as aerobic conditioning, agility training, and strength training.
Some of the greatest advice in preventing soccer injuries is to avoid overuse injuries. When it comes to the health of your body, more is not always better. Many sports medicine experts believe that it is helpful to take at least one season off each year. Although it’s hard, try to avoid the pressure that is now forced on many young athletes to over-train. Always listen to your body and decrease training time and intensity if pain or discomfort continues to increase. It will reduce the risk of injury and help avoid “burn-out.” Most injuries can be prevented to an extent. The last thing anyone wants to do is put an early end to his/her soccer career because they didn’t listen to their body and take care of themselves. As always, speak with a sports medicine professional if you have any concerns about injuries or soccer injury prevention strategies.
In order to keep kids and adults out on the field long-term and enjoy the sport of soccer, injury prevention, early detection, and treatment are significantly important.