Outer Hip Pain in Runners
Outer hip pain is a very common complaint we see with out runners at our Mission Valley office. The outer hip musculature is designed to provide hip, and lower back stabilization during running. When there is pain or tightness at the outer hip, the stability at the hip and lower back is compromised. This in turn can create abnormal stress into the hip, outer hip muscles, lower back, the knee, and even the lower leg/foot. The following conditions cause outer hip pain and dysfunction:
Causes of Outer Hip Pain
- Glute Medius Muscle Strain
- Tensor Fascia Latae Strain
- Gluteus Medius Tendinopathy
- Trochanteric Bursitis
- Iliotibial Tract Syndrome (IT Band Syndrome)
- Sciatic Nerve Entrapment
As mentioned above, the out hip plays a role in lower back and hip stability. If the outer hip is painful or dysfunctional the following conditions may also be present:
- Low Back Pain
- Facet Joint (Lower Back Joint) Irritation
- Hip Impingement
- Knee Tracking Issues
- Outer Knee Pain (IT Band Syndrome)
- Shin Splints
- Plantar Fasciitis
Evaluation
It is important to be evaluated by a running doctor and sports chiropractor. We will help diagnose your outer hip pain and any potential compensatory injuries that may be occurring simultaneously. A combination of range of motion, orthopedic, functional movements, and strength/endurance tests will be used to pinpoint the exact cause of your pain.
Gait Analysis
We currently offer at home gait analysis for current patients. After being evaluated in our office, if it is deemed necessary, we have our patients video tape themselves running on a treadmill and send it back to us for evaluation. For outer hip pain, many runners with outer hip pain run with what is known as a cross over gait. Check out our previous blog posts here on what a cross-over gait consists of.
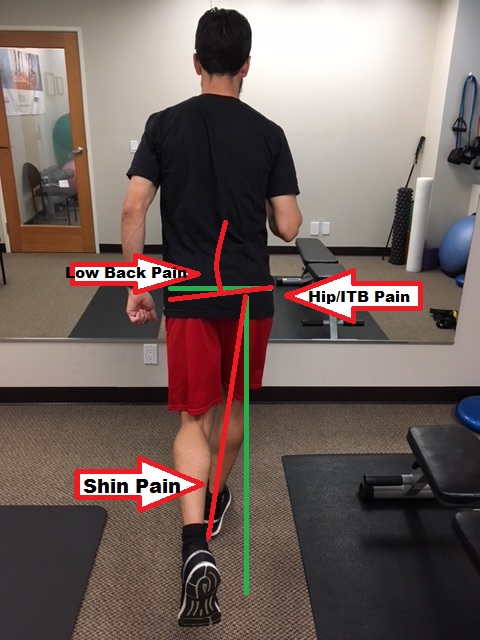
Potential sites for injury with cross over gait
Treatment for Outer Hip Pain
Active Release Technique is an excellent tool for helping runners with outer hip pain get out of pain quickly. A targeted home rehab approach is then prescribed b our running doctor as a way to prevent the injury from coming back again. Schedule with us today at our Mission Valley, San Diego running injury clinic today!












 In actuality, sitting with picture-perfect posture for long periods of time can actually lead to more discomfort, as it is extremely fatiguing. It can also lead to joint-pain and muscle strain because the torso is placing constant pressure on the lower disks in your back. Even in the ergonomically correct position, your arms and hands can still incur injuries. Any time you are sitting or standing in a static position, you increase the risk of prolonged physical conditions. To avoid any injuries at your workstation, try alternating between sitting and standing while working. Choose dynamic positions that will increase blood flow and alleviate stiff muscles. Also, include small rest breaks and stretch frequently to help avoid injuries.
In actuality, sitting with picture-perfect posture for long periods of time can actually lead to more discomfort, as it is extremely fatiguing. It can also lead to joint-pain and muscle strain because the torso is placing constant pressure on the lower disks in your back. Even in the ergonomically correct position, your arms and hands can still incur injuries. Any time you are sitting or standing in a static position, you increase the risk of prolonged physical conditions. To avoid any injuries at your workstation, try alternating between sitting and standing while working. Choose dynamic positions that will increase blood flow and alleviate stiff muscles. Also, include small rest breaks and stretch frequently to help avoid injuries.