Exercise to Combat Low back Pain in San Diego
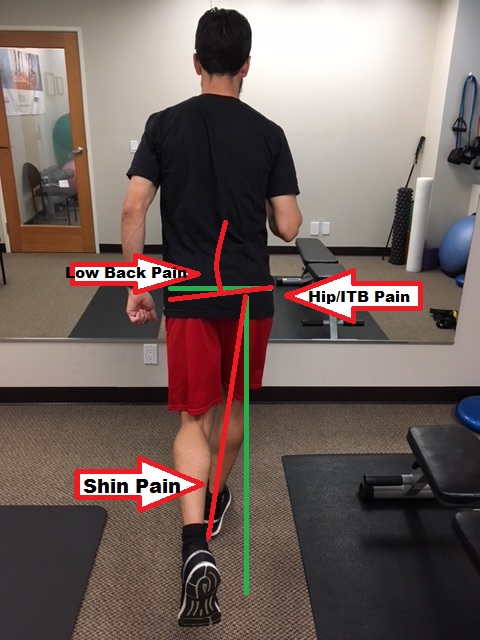
Low back pain is a painful, frustrating, and sometimes disabling condition. There are many different causes of low back pain (Different Types of Low Back Pain) but there are similar characteristics among back pain conditions that can be addressed to help address it. Common risk factors that are associated with low back pain are: Tall stature, obesity, weak core musculature, muscle imbalances, prior back injury, family members with low back pain, improper lifting or exercises mechanics. In our chiropractic office in Mission Valley, San Diego, near Pacific Beach, Ocean Beach, Hillcrest, and North Park, we see many types of low back pain. Majority of the time we need to address the functionality of the core. Many patients who are experiencing low back pain often carry their low backs in a disengaged position which causes hyperextension and irritation of the joints of the low back. This hyperextended position is often due to inhibition (inability to control) of the core musculature. By addressing this inhibition, patients begin to learn proper “lumbopelvic” control and posture, meaning they are able to hold their back in a stable position during their daily activities. The following low back exercise for low back pain, called the dead bug, is an excellent drill to utilize to teach patients how to use their deeper core musculature which is important in getting patients out of low back pain. The more control that is developed in these muscles, the more stable the back will be and less prone to causing pain.
“Dead Bug” Core Exercise
Start by laying on the ground with the legs bent 90 degrees at the knee and above the hip. Now, there should be an arch in the lower back or in other words, some space between the ground and the low back. Press the low back in towards the ground; this engages the deep abdominal and spinal core muscles. If you have pain when pressing down, try rolling up a towel about 1″ thick and place that under the low back for support. Hold the core engaged and slowly straighten one leg toward the ground about 6″ from the ground and back; repeat on the other leg. It is important to keep the back pressed toward the ground to develop the lower abdominal strength. Repeat this exercise, 3 x 10 nice and slow! If you can’t make it to 10 before you fatigue and the back arches, then stop on whatever rep it is that you maintain proper back position. Check out the video below for more details for the “dead bug” exercise.
If you are having low back pain, please get a full evaluation before attempting any new exercise routine. Back pain is complex and not all exercises work for every type of low back pain. Get a proper diagnosis with one of our sports chiropractors today. We are conveniently located in Mission Valley, San Diego. We are near the neighborhoods of La Jolla, UTC, Poway, Scripps Ranch, and Normal Heights. We are experienced in treating all types of low back pain!