Different Types of Low Back Pain
Common Causes of Low Back Pain
Low back pain is a very common issue experienced by the the general population at some point in life. Estimates vary but on average, about 38% of the general population experience low back pain in a year period.(2) Low back injury symptoms include: localized soreness, stiffness, and pain, radiating pain (pain into lower extremity), and possibly tingling and numbness into the lower extremity. The focus of this post will look at the common low back conditions we treat at our Mission Valley office.
First and foremost, we recommend seeking professional help from a certified sports chiropractor to correctly diagnose the low back injury. At our San Diego based sports injury clinic, we have seen many joint and disc injuries previously diagnosed as a “muscle strain” by a different provider. Simple diagnoses do patients no favors and will likely cause further harm!
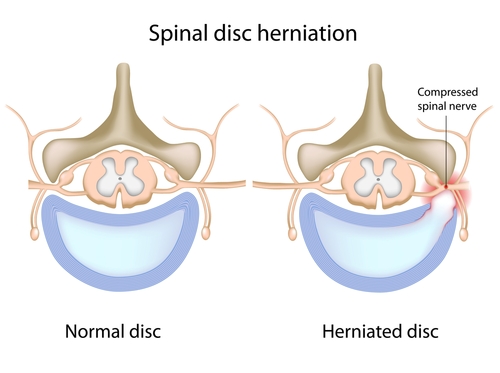
Disc Injury
Let’s start by discussing what I would consider the most time intensive injury to resolve. Disc injuries have the following characteristics: occur in younger people (20-40 year old), common in athletes, associated with a memorable mechanism of injury (squatted and felt a “pop” in back), recurring back injury, worse with bending forward, muscle spasming, pain in the back with cough/sneeze/bowel movement, may have radiating pain (sciatica), and may have numbness/tingling in the lower extremities.
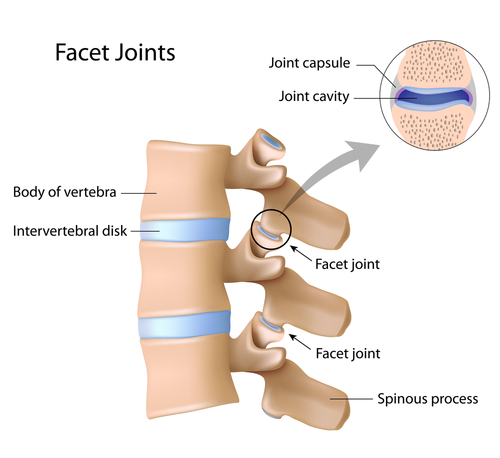
 Joint pain
Joint pain
Lower back joint pain is characterized by the following: occurs in middle aged to older individuals (40-65+) with no mechanism of injury (gradually worsened) or younger people with a mechanism of injury (football player tackled in low back), worse when bending backward, sharp localized pain in low back, muscle spasming, possible pain into buttocks/thigh. The image below shows healthy low back joints. They can be injured with hyper extension or excessive bending through the spine
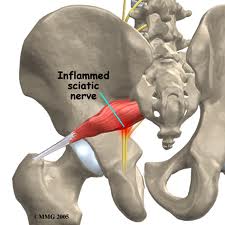
 Piriformis Syndrome
Piriformis Syndrome
Piriformis syndrome may be from acute spasming of the piriformis muscle (muscle runs from the tail bone to the outer hip) or from chronic tightening of the muscle. It is characterized by: pain in the buttocks, single sided sciatic symptoms, worse with sitting, no low back pain, worse with stretching hamstrings, and painful “knots” in the gluteal muscles/piriformis muscle. It is often misdiagnosed as a back related issue due to the symptoms of pain traveling down the leg. Check out our more thorough blog posts on piriformis syndrome found here: Piriformis Syndrome: Overview and Causes, Piriformis Syndrome Part II- Evaluation, and Piriformis Syndrome Part III- Treatment.
Low Back Muscle Strain
Please reread disc and joint causes of back pain. Both cause low back muscle spasming or muscles “locking up”. This is why doctors not certified to treat sport injuries diagnosis many low back injuries as a muscle strains. Technically they are not wrong because low back muscles are usually strained or spasmed when the deep structures (disc/joint) are injured. If you see a provider and they do not perform an evaluation including range of motion, orthopedic/neurological testing, and palpating (physically touching your back), get a second opinion. Once more serious conditions are ruled out, low back muscle strains are usually: local to the low back, muscle is sore/tight to touch, usually injured due to quick movements, and back muscles are often weak.
Special Types of Low Back Pain
Athletes with low back pain, especially in particular types of sports that involve repeated bending through the spine, may develop significant low back pain. Small fractures or stress reactions can occur to the pars interarticularis; a small portion of the vertebrea that when fracture can cause spondylolisthesis. Other injuries can involve the disc herniating into the end plate of the vertebral body of the low back. These types of injuries are confirmed with imaging (x-ray, MRI) but can be considered as a working diagnosis based on a thorough history and physical exam. If you have a sport related low back pain, please get evaluated by one of our Mission Valley sports chiropractors.
Treatment
In a recent review article discussing conservative management of low back pain, several methods are described as primary treatment choices for acute and chronic low back pain. For acute low back pain, chronic low back pain, and chronic low back pain with leg pain, a trial of spinal manipulative therapy with supplementary treatments such as exercise, massage, and patient education is recommended.(1) Specific types of exercises are prescribed based on the practitioner’s experience and patient’s tolerance. In other words, each person with low back pain may receive different exercises based on their presenting symptoms. Decreased pain and symptoms we found after short term (1-3 months) and long term (6-12 months) follow ups.
Initial treatment for low back pain is recommended between 4-8 visits over a 4 week period. (1)

At our office in Mission Valley, we customize treatment plans for each and every low back pain patient we see. For example, if a patient has a diagnosed disc injury in their back, extension based exercises for the low back may offer significant relief for one patient, yet cause terrible pain in the next patient with the exact diagnosis. Evaluation in person by a certified sports chiropractor will be able to determine the correct treatment approach. We utilize the latest techniques including spinal manipulative therapy, Active Release Technique, Graston Technique, and rehabilitative exercise.
References
Brussieres, A. E. et al. (2018). Spinal manipulative therapy and other conservative treatments for low back pain: a guideline from the canadian chiropractic guideline initiative. Journal of Manipulative and Physiological Therapeutics. 0 (0), 1-29.
Hoy, D. et al. (2010). The epidemiology of low back pain. Best Practice and Research Clinical Rheumatology. 24 (5), 769-781.