Is Running BAD for your discs?
/in Low Back Pain, Low back Sports Injury, running injury, Uncategorized/by adminRunning and Your Spine: A New Look at Intervertebral Disc Health
There’s a common myth that running is bad for your back. But a new systematic review published in Sports Health tells a different story. This review combined 13 studies with 632 participants to investigate how running affects the health of intervertebral discs—the cushions between the vertebrae in your spine.
How Running Affects Your Spine
The review looked at two types of studies: some measured how running affected spinal height, while others used MRI to observe changes in disc composition. Here’s what the research found:
- Temporary Compression: Running causes temporary compression of the discs. This means that during a run, discs lose some water content and slightly shrink in height.
- Supercompensation Between Runs: After the run, your discs supercompensate by drawing water and glycosaminoglycans back in. These are important for keeping your discs hydrated and healthy. Over time, this process can actually improve disc health.
- Stronger, Healthier Discs: Habitual runners were found to have healthier and stronger discs than non-runners. So rather than damaging your spine, regular running appears to build resilience in your intervertebral discs.
Takeaways for Runners
This study is great news for runners and those hesitant to start due to back pain concerns. Here’s what you should know:
- Running is Safe for Your Back: The temporary disc compression during a run is completely normal and healthy. The key is the recovery between runs, where your body replenishes lost fluids and nutrients.
- Regular Running Builds Stronger Discs: Over time, the cycles of compression and supercompensation make your discs more resilient, reducing the risk of spinal issues.
- No Need to Fear Running: If you’ve been avoiding running due to fears of back injury, this study shows that running is not only safe but can actively improve your spinal health.
Incorporating regular runs into your routine can be a powerful way to maintain a healthy back. So, lace up those running shoes and start reaping the benefits for your spine!
Reference: Shu D, Dai S, Wang J, Meng F, Zhang C, Zhao Z. Impact of Running Exercise on Intervertebral Disc: A Systematic Review. Sports Health. 2024;0(0). doi:10.1177/19417381231221125
Facet Joint Syndrome and Pain
/in Headaches, Low Back Pain, Neck Pain/by adminSome of the links on this page regarding facet joint syndrome and pain are affiliate links. We may receive a small commission if you choose to click the link and purchase an item. By clicking, you are helping our small business and we thank you! We only link to products we believe in and use regularly with our patients.
Facet Joint Syndrome Overview
Facet joint syndrome can be a significant source of back and neck pain. It is caused by irritation of the joints between the vertebrae on the back side of the spine. The facet joint can become inflamed from a variety of causes such as a bad night’s sleep, prolonged poor posture, awkward lifting and others. When the joint gets irritated it triggers pain signals in nearby nerve endings.
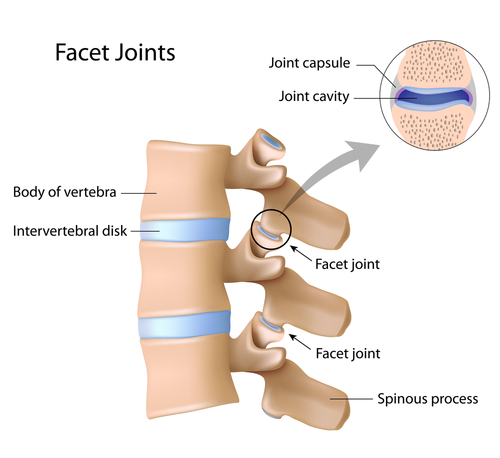
Anatomy of the Facet Joints
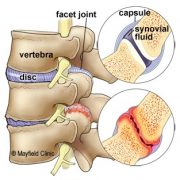
The spine is made of a column of moveable bones called vertebrae that connect to one another. Each vertebra functions as a three-joint complex with a large disc in the front and two facet joints in the back. This tripod design is strong, keeping the bones linked together while allowing our spine to bend and twist. Facets are synovial joints that are lined with cartilage, lubricated in synovial fluid and covered by a joint capsule. Healthy facet joints glide and slide as the back moves, but prevent over-twisting.
Figure 1. Side view of the spine shows a normal disc and facet joint (top). Irritation to the disc and facet joint syndrome can cause arthritic pain, swelling and stiffness (bottom).
In Facet joint syndrome, the facets get inflamed which causes pain and loss of motion in the joint. In turn, the muscles in the area can stiffen and spasm leading to further pain and decreased motion.
Figure 2. The irritated joint sends pain signals to the brain via small nerves in the capsule called medial branch sensory nerves
What are the Symptoms of Facet Syndrome?
There are several symptoms that indicate a person’s pain is coming from the facet joints. The pain is often a diffuse, dull ache in the neck or in the shoulder blade area. Often people describe the pain as a sharp, pinching, catching or a “crick” in their neck.
Movements such as looking up or turning your head side to side especially towards the affected joint will often cause pain. Facet joint symptoms may also mimic the pain of a disc herniation. If the inflammation irritates the spinal nerves, pain may be felt down the extremity. The pain may be chronic, or come in periodic flare-ups.
How is a Diagnosis of Made?
Different movements through the injured area and pointing to the painful area help with the working diagnosis. The doctor may manipulate your joints or feel for tenderness over the spine. In some cases, imaging studies, such as X-ray, CT, or MRI, may be ordered to help in the diagnosis. Imaging can help rule out other pathology of the spine, shoulders, hip, etc. which may be causing the symptoms.
What Treatments are Available?
Chiropractic adjustments are effective in relieving the pain from facet joint syndrome. In fact, the sound of that is made when your spine is adjusted is actually gas escaping from the facet joints which leads to decreased pressure and improved movement. Traction of the head and neck is also effective for the same reason as adjustments in that it helps to open the facet joints and decrease the pressure that is creating pain.
Active Release techniques (ART) are deep tissue muscular treatments that help relieve tightness and spasm surrounding the irritated facet joint. By decreasing muscle tension around the facet joints, adjustments are much more easily performed.
Home Exercise Therapy
After treatment, targeted stretches and exercises are important to perform daily while recovering. Towel neck mobilization exercises are one of the best types of exercises for facet syndrome. This exercise (as shown below) uses a towel to create a fulcrum for the spine to bend over. This allows the facet joint to remain open as you move; we often see people that can barely look up without pain quickly gain pain free motion by performing this exercise.
Stretching encouraging flexion of the neck as shown in the video below is helpful. Rotational mobilization may be helpful as well. In acute injury, this is often too aggressive but as the neck heals, the neck rotational exercise can be very beneficial.
Cervical Spine Devices
At home traction devices are a great at home treatment option. Inflatable neck traction devices are easy to use and you can take them anywhere with you. The Neck Hammock is an easy to use system that only requires a door handle to use. The absolute best neck traction device is the Saunders Pneumatic Traction device. It is bulky but is ale to deliver substantial traction to the neck joints.
Lumbar Spine Devices
For lumbar spine traction, there are two devices that we find most useful. The first and most commonly known is an inversion table. The Teeter Inversion Table is one of the best and most reliable inversion tables. As with all inversion tables, they take up quite a bit of space and are not easily moveable. The second device is the Back Bubble. This is a convenient alternative to an inversion table. You need a place to hang it from, a doorway pull-up bar is the easiest. Not only does this device work well, you can put it away when you are done using it! You do not need permanent space in your home like the inversion table.
Day to Day Self Care
Self care is an important component of care for facet pain in the neck. Using correct posture and keeping your spine in alignment are important things you can do to prevent painful episodes. You may need to make adjustments to your daily standing, sitting, and sleeping habits. Light cardiovascular exercise like walking or riding a bike is very helpful for a painful facet joint, and it can help you heal faster. Facet joint pain usually resolves after 4-6 treatments over the course of 1-3 weeks.
Recovery and Prevention
Regular stretching, strengthening, postural awareness, and cardiovascular exercise reduces stress to the facet joints. Facet pain can be recurrent and in some cases lead to chronic neck pain if not treated effectively and cared for by making long term preventative changes.
Dr. Kevin and Travis Rose DC are chiropractors trained in treating overuse and sport related injury. Peak Form Health Center is located in Mission Valley, San Diego near the neighborhoods of La Jolla, Mission Hills, Kensington, and Carmel Valley. Schedule an appointment with use by using “Schedule Now” tab at the top of this page, or call 619-818-4306.
Low Back Pain Exercises
/in Back Pain Prevention, Low Back Pain, Low back Sports Injury/by Dr. Travis RoseMany people experience low back pain each year. Because the low back is a complex structure of joints, discs, ligaments, and muscles, the source of pain can be tricky to determine. Low back pain exercises are a must to help with the healing process and decrease your risk for a future injury.
Starting patients off with low back pain exercises, we like to address the back and hip tissue tightness, and mobility. In most cases of low back pain, the muscles of the back and hip develop trigger points. Trigger points are focal areas of hypersensitive fibers that cause local pain and refer pain. Performing low back pain exercises that target these tight spots can have significant effect at decreasing symptoms.
Here are our favorite low back pain exercises to help address tight, sore muscles in the back and hip.
Low Back Pain Exercises: Self Massage Technique
A massage ball to the lower back can be very effective at loosening your the lower back muscles. We like lacrosse balls as they are very firm and easily press into the low back muscles. Some people with smaller or thin body types may find the lacrosse ball to be too uncomfortable. Tennis ball, or racquet ball may work better.
Here is a nice video demonstration on how to perform lower back self massage.
Gluteal Self Massage
The second of the low back pain exercises we like to prescribe is self massage for the gluteal muscles. Again we like a lacrosse ball as it gets deep into the dense hip musculature. Try this one out on the wall. You can easily control the pressure from the ball and access different angles into the muscles easily. This exercise is also excellent in managing Iliotibial Band Syndrome.
Child’s Pose
An easy, but effective exercise to help with low back pain, stiffness, and tightness. This one of the more gentle low back pain exercises. It simultaneously stretches the low back muscles, while decompressing the low back joints and discs. Our video shows how to perform Child’s pose on multiple directions.
Lower Back Pain Decompression Exercise
Many people have heard of inversion tables to help take pressure of the low back. They are absolutely effective for many types of low back pain but they are expensive and they take up a lot of room. The decompression stretch below, utilizes a Swiss ball to provide a fulcrum which helps take pressure off the lumbar spine. You must be very relaxed when performing this exercise. You should not experience any pain with it at all
Low back pain exercises are a must in any treatment protocol for the low back. We start patients with exercises on the first day of treatment for the best outcomes. If you are in need of an evaluation and treatment, please schedule with us today! We are conveniently located in Mission Valley, San Diego near the neighborhoods of La Jolla, Carmel Valley, Mission Hills, Hillcrest, and Bird Rock.
Drs Travis and Kevin Rose are sports chiropractors in San Diego, California. They treat a wide range of injuries and have helped thousands of patients get back to their potential. Athletes themselves, they understand the importance of recovering from injury and returning to sport.
Sciatica- Conservative Management San Diego
/in Conditions, Low Back Pain/by adminSciatica is a term that encompasses any condition that that can effect the sciatic nerve. Low back and hip injuries are the most common types of injuries that produce sciatica or sciatic symptoms. Less commonly, peripheral entrapment of the nerve around the hamstrings, and lower leg muscles cause sciatica symptoms in the back of the leg. Our San Diego chiropractor at Peak Form Health Center has treated countless conditions that cause sciatica symptoms.
What causes Sciatic Symptoms?
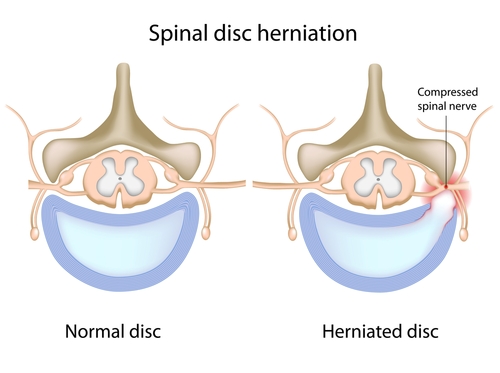
The sciatic nerve is made up of many different nerve roots from the low back and sacrum (tail bone). The nerve roots are extensions from the spinal cord that exit the spine to form peripheral nerves (ex: sciatic nerve is a peripheral nerve). If you have a back injury like a disc bulge, the disc bulge can press on the exiting nerve root which causes nerve irritation. Nerve irritation symptoms can cause numbness, tingling, hot/cold sensations, shooting pain, loss of sensation, and/or loss of function to the muscles that nerve innervates. Those same symptoms are what are described as “sciatica” but typically patients refer to sharp shooting pain as sciatica. Other conditions that can cause sciatica are:
- Low back injury- See our post on types of low back pain here: Different Types of Low Back Pain
- Disc bulge
- Disc herniation
- Piriformis syndrome– see our thorough blog post on piriformis syndrome here: Piriformis Syndrome: Overview and Causes Piriformis Syndrome Part II- Evaluation Piriformis Syndrome Part III- Treatment
- Degenerative Disc Disease
- Degenerative Joint Disease
- Foraminal stenosis of the lumbar spine (Bone Spurring)
- Central canal stenosis
- Sciatic nerve entrapment
- Spondylolisthesis
In rare but serious cases, sciatic symptoms may be due to: tumors, infection, tethered spinal cord, and other neurological conditions.
Conservative Management for Sciatica
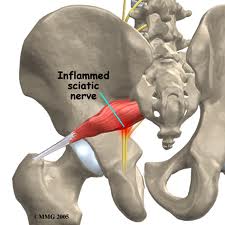
First and foremost, a proper diagnosis is required to treat your symptoms effectively. Depending on what the cause is and how long it has been going on, usually a combination of manual therapy, specific exercise protocols, and home education can help resolve sciatica. Let’s take piriformis syndrome as an example. In piriformis syndrome, the piriformis muscles compresses the sciatic nerve. To treat this, targeted Active Release Techique and other myofascial release techniques often results in drastic improvement of symptoms. If however, the sciatica is due to a low back condition, manual therapy to the piriformis muscle will likely not result in significant relief of symptoms.
To reiterate the first point, it is important to see a sports chiropractor or sports medicine professional who will accurately diagnose what is causing the sciatica. Many times we see patients who have been dealing with sciatic symptoms for months and have been doing self treatments that are actually perpetuating their symptoms. Be very wary of a “do this one thing for your sciatica.” type blog post as it may be causing more harm than good.
Our San Diego based chiropractic group treats many different causes of sciatic symptoms. If there is ever concern of a more serious condition causing sciatica, or further investigation is required, we will make an appropriate referral to get the best care for you. Schedule today to get a thorough evaluation. Our office is conveniently located in Mission Valley, San Diego.
Different Types of Low Back Pain
/in Low Back Pain, Low back Sports Injury, Sports Injury/by adminCommon Causes of Low Back Pain
Low back pain is a very common issue experienced by the the general population at some point in life. Estimates vary but on average, about 38% of the general population experience low back pain in a year period.(2) Low back injury symptoms include: localized soreness, stiffness, and pain, radiating pain (pain into lower extremity), and possibly tingling and numbness into the lower extremity. The focus of this post will look at the common low back conditions we treat at our Mission Valley office.
First and foremost, we recommend seeking professional help from a certified sports chiropractor to correctly diagnose the low back injury. At our San Diego based sports injury clinic, we have seen many joint and disc injuries previously diagnosed as a “muscle strain” by a different provider. Simple diagnoses do patients no favors and will likely cause further harm!
Disc Injury
Let’s start by discussing what I would consider the most time intensive injury to resolve. Disc injuries have the following characteristics: occur in younger people (20-40 year old), common in athletes, associated with a memorable mechanism of injury (squatted and felt a “pop” in back), recurring back injury, worse with bending forward, muscle spasming, pain in the back with cough/sneeze/bowel movement, may have radiating pain (sciatica), and may have numbness/tingling in the lower extremities.
 Joint pain
Joint pain
Lower back joint pain is characterized by the following: occurs in middle aged to older individuals (40-65+) with no mechanism of injury (gradually worsened) or younger people with a mechanism of injury (football player tackled in low back), worse when bending backward, sharp localized pain in low back, muscle spasming, possible pain into buttocks/thigh. The image below shows healthy low back joints. They can be injured with hyper extension or excessive bending through the spine
 Piriformis Syndrome
Piriformis Syndrome
Piriformis syndrome may be from acute spasming of the piriformis muscle (muscle runs from the tail bone to the outer hip) or from chronic tightening of the muscle. It is characterized by: pain in the buttocks, single sided sciatic symptoms, worse with sitting, no low back pain, worse with stretching hamstrings, and painful “knots” in the gluteal muscles/piriformis muscle. It is often misdiagnosed as a back related issue due to the symptoms of pain traveling down the leg. Check out our more thorough blog posts on piriformis syndrome found here: Piriformis Syndrome: Overview and Causes, Piriformis Syndrome Part II- Evaluation, and Piriformis Syndrome Part III- Treatment.
Low Back Muscle Strain
Please reread disc and joint causes of back pain. Both cause low back muscle spasming or muscles “locking up”. This is why doctors not certified to treat sport injuries diagnosis many low back injuries as a muscle strains. Technically they are not wrong because low back muscles are usually strained or spasmed when the deep structures (disc/joint) are injured. If you see a provider and they do not perform an evaluation including range of motion, orthopedic/neurological testing, and palpating (physically touching your back), get a second opinion. Once more serious conditions are ruled out, low back muscle strains are usually: local to the low back, muscle is sore/tight to touch, usually injured due to quick movements, and back muscles are often weak.
Special Types of Low Back Pain
Athletes with low back pain, especially in particular types of sports that involve repeated bending through the spine, may develop significant low back pain. Small fractures or stress reactions can occur to the pars interarticularis; a small portion of the vertebrea that when fracture can cause spondylolisthesis. Other injuries can involve the disc herniating into the end plate of the vertebral body of the low back. These types of injuries are confirmed with imaging (x-ray, MRI) but can be considered as a working diagnosis based on a thorough history and physical exam. If you have a sport related low back pain, please get evaluated by one of our Mission Valley sports chiropractors.
Treatment
In a recent review article discussing conservative management of low back pain, several methods are described as primary treatment choices for acute and chronic low back pain. For acute low back pain, chronic low back pain, and chronic low back pain with leg pain, a trial of spinal manipulative therapy with supplementary treatments such as exercise, massage, and patient education is recommended.(1) Specific types of exercises are prescribed based on the practitioner’s experience and patient’s tolerance. In other words, each person with low back pain may receive different exercises based on their presenting symptoms. Decreased pain and symptoms we found after short term (1-3 months) and long term (6-12 months) follow ups.
Initial treatment for low back pain is recommended between 4-8 visits over a 4 week period. (1)

At our office in Mission Valley, we customize treatment plans for each and every low back pain patient we see. For example, if a patient has a diagnosed disc injury in their back, extension based exercises for the low back may offer significant relief for one patient, yet cause terrible pain in the next patient with the exact diagnosis. Evaluation in person by a certified sports chiropractor will be able to determine the correct treatment approach. We utilize the latest techniques including spinal manipulative therapy, Active Release Technique, Graston Technique, and rehabilitative exercise.
References
Brussieres, A. E. et al. (2018). Spinal manipulative therapy and other conservative treatments for low back pain: a guideline from the canadian chiropractic guideline initiative. Journal of Manipulative and Physiological Therapeutics. 0 (0), 1-29.
Hoy, D. et al. (2010). The epidemiology of low back pain. Best Practice and Research Clinical Rheumatology. 24 (5), 769-781.
PEAK FORM NEWSLETTER SIGN UP
Our Office