Posts
Strengthening Bones with High Velocity Resistance Training (HVRT): A Guide for Those with Osteopenia and Osteoporosis
/in Bone Density, Training/by adminStrengthening Bones with High Velocity Resistance Training (HVRT): A Guide for Those with Osteopenia and Osteoporosis
For anyone managing osteopenia or osteoporosis, finding safe, effective ways to protect and strengthen bone health is critical. A recent systematic review, focused on high velocity resistance training (HVRT), provides valuable insights on how this type of training can benefit bone mineral density (BMD) in older adults—particularly at the lumbar spine, hip, and femoral neck, which are key areas prone to fractures.
What is HVRT?
High velocity resistance training (HVRT) is a form of exercise that combines speed with strength, emphasizing powerful, controlled movements that target muscle and bone. Unlike traditional resistance training, HVRT often involves quicker concentric (lifting) movements paired with slower eccentric (lowering) movements, which engage the muscles attached to bones in ways that promote bone health.
Key Findings from the Review
This review included 25 studies, totaling over 1,200 participants. Here’s what it found:
- Small but Significant Gains in Bone Density: The review found that HVRT programs, when performed twice or more weekly, had a significant positive impact on BMD in older adults. Increases ranged from 0.9% to 5.4%, primarily in the lumbar spine, femoral neck, and total hip.
- Consistency is Crucial: Importantly, studies showed that BMD improvements were lost if exercise was stopped for six months or longer. Thus, consistency is essential to maintaining gains.
- Multimodal Programs Enhance Outcomes: Programs that combined HVRT with other exercises, such as balance and flexibility work, tended to show even better results. This blend of exercises seems to create a synergistic effect that further supports bone density.
- Longer Duration Leads to Better Results: Programs lasting six months or more tended to yield the most notable BMD improvements. Bone remodeling is a slow process, so longer-term commitments to HVRT are recommended.
Practical Takeaways for Improving Bone Health
1. Consider HVRT as Part of Your Routine
- Minimum Frequency: Aim for at least two HVRT sessions per week.
- Duration: Commit to at least six months of consistent training to see meaningful changes in bone density.
- Controlled Environment: HVRT is best done in a safe, supervised setting, such as with a trainer experienced in osteoporosis-friendly exercise regimens, especially for those new to resistance training.
2. Blend HVRT with Other Exercises
- Including balance exercises, flexibility work, and moderate-impact activities (like walking or light jogging) can amplify the osteogenic effects of HVRT, helping to strengthen not only bones but also the muscles and ligaments supporting them.
3. Avoid Long Breaks
- If you stop training for six months or more, you risk losing any gains in BMD. Schedule your workouts as part of your weekly routine, and avoid long gaps to maintain bone strength.
Making It Work for You: Safety First
For many, the idea of high velocity training can sound intimidating, especially if you’re managing a condition like osteoporosis. However, HVRT can be modified with machines or lighter weights to accommodate different ability levels safely. Additionally, explosive movements can be adjusted to fit your fitness level—there’s no need to engage in highly intense or Olympic-style lifting to benefit from HVRT.
Beyond Bone Health: Preventing Sarcopenia and Powerpenia
Alongside improving BMD, HVRT may also help prevent sarcopenia (age-related muscle loss) and powerpenia (decline in muscle power). Sarcopenia and powerpenia are serious issues for older adults, leading to reduced mobility, higher fall risk, and overall decreased quality of life. HVRT, with its focus on explosive movements, can help retain both muscle mass and power, essential for everyday tasks and fall prevention.
For more on powerpenia read our full article here.
Take Control of Your Bone Health
For those diagnosed with osteopenia or osteoporosis, HVRT offers a promising, science-backed way to take control of bone health. Start by consulting with your healthcare provider and a qualified trainer who can help design a safe, effective HVRT program tailored to your needs. With commitment and the right guidance, you can build a sustainable exercise routine that strengthens your bones and supports long-term health.
Let’s build stronger bones—starting today!
C
REFERENCE: Haque, I., Schlacht, T. Z., & Skelton, D. A. (2024). The effects of high velocity resistance training on bone mineral density in older adults: A systematic review. Bone, 179, 116986. https://doi.org/10.1016/j.bone.2023.116986
3 Food Products That Supercharge Recovery: Tart Cherry Juice, Watermelon, and Pineapple
/in Tips/by adminFacet Joint Syndrome and Pain
/in Headaches, Low Back Pain, Neck Pain/by adminSome of the links on this page regarding facet joint syndrome and pain are affiliate links. We may receive a small commission if you choose to click the link and purchase an item. By clicking, you are helping our small business and we thank you! We only link to products we believe in and use regularly with our patients.
Facet Joint Syndrome Overview
Facet joint syndrome can be a significant source of back and neck pain. It is caused by irritation of the joints between the vertebrae on the back side of the spine. The facet joint can become inflamed from a variety of causes such as a bad night’s sleep, prolonged poor posture, awkward lifting and others. When the joint gets irritated it triggers pain signals in nearby nerve endings.
Anatomy of the Facet Joints
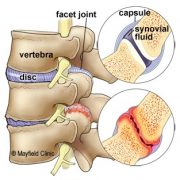
The spine is made of a column of moveable bones called vertebrae that connect to one another. Each vertebra functions as a three-joint complex with a large disc in the front and two facet joints in the back. This tripod design is strong, keeping the bones linked together while allowing our spine to bend and twist. Facets are synovial joints that are lined with cartilage, lubricated in synovial fluid and covered by a joint capsule. Healthy facet joints glide and slide as the back moves, but prevent over-twisting.
Figure 1. Side view of the spine shows a normal disc and facet joint (top). Irritation to the disc and facet joint syndrome can cause arthritic pain, swelling and stiffness (bottom).
In Facet joint syndrome, the facets get inflamed which causes pain and loss of motion in the joint. In turn, the muscles in the area can stiffen and spasm leading to further pain and decreased motion.
Figure 2. The irritated joint sends pain signals to the brain via small nerves in the capsule called medial branch sensory nerves
What are the Symptoms of Facet Syndrome?
There are several symptoms that indicate a person’s pain is coming from the facet joints. The pain is often a diffuse, dull ache in the neck or in the shoulder blade area. Often people describe the pain as a sharp, pinching, catching or a “crick” in their neck.
Movements such as looking up or turning your head side to side especially towards the affected joint will often cause pain. Facet joint symptoms may also mimic the pain of a disc herniation. If the inflammation irritates the spinal nerves, pain may be felt down the extremity. The pain may be chronic, or come in periodic flare-ups.
How is a Diagnosis of Made?
Different movements through the injured area and pointing to the painful area help with the working diagnosis. The doctor may manipulate your joints or feel for tenderness over the spine. In some cases, imaging studies, such as X-ray, CT, or MRI, may be ordered to help in the diagnosis. Imaging can help rule out other pathology of the spine, shoulders, hip, etc. which may be causing the symptoms.
What Treatments are Available?
Chiropractic adjustments are effective in relieving the pain from facet joint syndrome. In fact, the sound of that is made when your spine is adjusted is actually gas escaping from the facet joints which leads to decreased pressure and improved movement. Traction of the head and neck is also effective for the same reason as adjustments in that it helps to open the facet joints and decrease the pressure that is creating pain.
Active Release techniques (ART) are deep tissue muscular treatments that help relieve tightness and spasm surrounding the irritated facet joint. By decreasing muscle tension around the facet joints, adjustments are much more easily performed.
Home Exercise Therapy
After treatment, targeted stretches and exercises are important to perform daily while recovering. Towel neck mobilization exercises are one of the best types of exercises for facet syndrome. This exercise (as shown below) uses a towel to create a fulcrum for the spine to bend over. This allows the facet joint to remain open as you move; we often see people that can barely look up without pain quickly gain pain free motion by performing this exercise.
Stretching encouraging flexion of the neck as shown in the video below is helpful. Rotational mobilization may be helpful as well. In acute injury, this is often too aggressive but as the neck heals, the neck rotational exercise can be very beneficial.
Cervical Spine Devices
At home traction devices are a great at home treatment option. Inflatable neck traction devices are easy to use and you can take them anywhere with you. The Neck Hammock is an easy to use system that only requires a door handle to use. The absolute best neck traction device is the Saunders Pneumatic Traction device. It is bulky but is ale to deliver substantial traction to the neck joints.
Lumbar Spine Devices
For lumbar spine traction, there are two devices that we find most useful. The first and most commonly known is an inversion table. The Teeter Inversion Table is one of the best and most reliable inversion tables. As with all inversion tables, they take up quite a bit of space and are not easily moveable. The second device is the Back Bubble. This is a convenient alternative to an inversion table. You need a place to hang it from, a doorway pull-up bar is the easiest. Not only does this device work well, you can put it away when you are done using it! You do not need permanent space in your home like the inversion table.
Day to Day Self Care
Self care is an important component of care for facet pain in the neck. Using correct posture and keeping your spine in alignment are important things you can do to prevent painful episodes. You may need to make adjustments to your daily standing, sitting, and sleeping habits. Light cardiovascular exercise like walking or riding a bike is very helpful for a painful facet joint, and it can help you heal faster. Facet joint pain usually resolves after 4-6 treatments over the course of 1-3 weeks.
Recovery and Prevention
Regular stretching, strengthening, postural awareness, and cardiovascular exercise reduces stress to the facet joints. Facet pain can be recurrent and in some cases lead to chronic neck pain if not treated effectively and cared for by making long term preventative changes.
Dr. Kevin and Travis Rose DC are chiropractors trained in treating overuse and sport related injury. Peak Form Health Center is located in Mission Valley, San Diego near the neighborhoods of La Jolla, Mission Hills, Kensington, and Carmel Valley. Schedule an appointment with use by using “Schedule Now” tab at the top of this page, or call 619-818-4306.
Top Tips to Treat Tennis Elbow at Home
/in Sports Injury, Tips/by adminSome of the links in this post are affiliate links. We may earn an affiliate commission if you click on a link and purchase an item we recommend. This doesn’t add any additional cost to you, but helps support our business.
When you treat tennis elbow at home it will often help significantly reduce the amount of time this painful condition persists. At home, using a combination of pain relieving gels, taping/strapping, myofascial release, and specific exercises, tennis elbow will improve.
Lateral epicondylitis, or more commonly “Tennis Elbow”, is a painful tendinopathy that affects the outer elbow. It is considered an over-use injury to the extensor muscles of the forearm. The extensor muscles of the forearm connect into a common tendon which inserts into the bony part of the outer elbow. With excessive use the muscles tighten and pull at the outer elbow. Pain can be sharp, achy, and fairly constant.
*The following tips are general recommendations. We highly recommend seeking the advice of a qualified healthcare provider to provide a diagnosis and proper treatment plan.
Common Causes of Tennis Elbow are as follows:
- Playing tennis
- Excessive computer use (typing)
- Rock Climbing
- Repetitive wrenching (mechanics, plumbers)
- Jiu Jitsu
- Excessive weight training
Tips to Treat Tennis Elbow at Home
- Armaid Foam Massage Tool
– The Armaid
is a self myofascial release tool designed to break down tight muscles of the forearm. It comes with a number of different attachments to isolate myofascial adhesions (scar tissue) and break them down. With consistent use, the muscles will begin to regain their normal flexibility which will relieve pressure from the painful elbow insertion. This device, in our opinion, is one of the best devices you can use for treating tennis elbow at home. It is especially useful if you participate in a job/sport that causes a lot of strain into the forearm muscles.
This device is excellent not only for treating tennis elbow at home but for treating “Golfer’s Elbow” which affects the opposite side of the elbow. Watch Dr. Rose demonstrate how to use the Armaidin our video below.
- TheraBand FlexBar, Tennis Elbow Therapy
– The FlexBar
is a flexible bar with grip ridges that allows the bar to twist. The exercise performed is an eccentric load to the extensor muscle group of the forearm. Eccentric loading has been shown in research to strengthen damaged tendons and stretch the muscle fibers. The FlexBar
accomplishes this by having the patient grab the bar with the wrist down, and twist the bar up so the wrist is now up. Slowly release to perform the eccentric contraction. Watch Dr. Rose demonstrate this treatment for tennis elbow at home. It can be a little confusing when you start!
- RockTape
– RockTape is a brand of kinesiology tape. It is designed to support muscle strains, joint sprains, and proper movement mechancis. To treat Tennis Elbow at home, it helps by supporting the extensor muscle group, and the cross strap before the elbow, helps absorb forces from traveling to the painful point on the elbow.

We prefer rock tape for one simple reason, it just seems to stick better than other brands. It can also be used in conjunction with RockTape’s Rock Sauce Hotand RockSauce Ice, depend if you prefer hot or cold sensations. You put RockSauce on first to which helps remove oils from the skin and you get the benefit of pain relieving effects of hot or cold sensations. You can then apply the Rocktape to the same area.
Biofreeze Pain Relief Gel
– Another option to RockSauce. We recommend Biofreeze Pain Relief Gel as it is one of the stronger topical pain relieving gels you can get. It is a product we use daily in our office and can be great for treating tennis elbow at home. Just apply a dime sized portion all around the elbow to help with pain.
- Simien Tennis Elbow Brace– A Tennis Elbow Brace can work well for in a couple different scenarios. First, when Tennis Elbow is affecting day to day activities such as opening doors, cooking, shaking hands. Second, when you still need to train or compete at a high level for a competition. The brace works by compressing the tendon right before the insertion point which is the most painful. When forces travel up the forearm, they get dispersed at the site of the brace, minimizing the amount of force that travels all the way to the painful point. Ideally, we want to treat and work tennis elbow to get rid of the symptoms, but this works well to treat tennis elbow at home when dealing with pain.
- Muscle Floss AKA Voodoo Floss– Muscle Flossing is a relatively new treatment method for various conditions. It can be a great too to treat Tennis Elbow at home. Muscle flossing works through ischemic compression with rapid blood release into the injured area.
To explain further, you tightly wrap the elastic band around the elbow. You want to the band to be pretty tight to where it is mildly challenging to bend the elbow. For 30-60 seconds, bend then elbow back and forth, and move the wrist up and down. The band restricts blood flow to the area and movement pumps blood out of the area. You then rapidly release the band which releases rapid blood flow to the area.
The idea is, this rapid injection of blood to the injured area will help increase the healing process to the tissue. In the pictures below, you can see the elbow is red due to blood flow after 30 seconds of elbow motion.


Those were the top tips we give to patients to help treat tennis elbow at home. We recommend these tips with in person treatment to help fix tennis elbow effectively and quickly. Countless cases of tennis elbow have been treated in our Mission Valley, San Diego office. We primarily use Active Release Techinque, Graston Technique, exercises and a combination of the above tips to treat tennis elbow at our office. Our office is near the neighborhoods of Pacific Beach, UTC, La Jolla, Clairemont Mesa, Santee, La Mesa, Kensington, North Park and South Park.
Runner’s Knee Treatment |San Diego
/in running form, running injury, Sports Injury/by adminRunner’s Knee Treatment | San Diego
Patellofemoral pain syndrome, aka runner’s knee, is characterized by achy, dull pain generally around the front of the knee. Runner’s knee is a common type of running injury that we see in our San Diego running injury clinic. With a combination of manual therapy, exercise, and run program modification, the runner returns to running pain free. Let’s take a look at common symptoms/causes of runner’s knee and the treatments that will get you back to running pain free.
Symptoms
Most runners will feel dull, achy pain diffusely around the front of the knee. The pain may favor the outer front or the inner front of the knee. It is usually worse with longer or down hill runs. Sitting for long periods usually increases tightness and soreness around the knee. Stretching often makes the knee feel better.

Common Causes of Runner’s Knee
Here are the most common causes for developing runner’s knee.
- Running Form– Many runners, beginner through experienced, have running form flaws that create excessive tension at the knees. Common culprits are running with a low cadence, over striding, running with a crossover gait, and poor posture. Read our blogs for more information: Increase Your Cadence!, Do You Run With a Cross-Over Gait?, Improve Running Posture.
- Performing “Too much, Too Soon”– This is what most commonly affects newer runners. They begin training for their first 5k, 10k, or half marathon and start running too many miles with too little recover. The tissues do not have enough time to heal between running sessions, and eventually injury results.
- Training Error– If a runner drastically changes their training, runner’s knee can develop. Adding significant amounts of hill training, particularly running down hill, is the most common training error that can cause or exacerbate runner’s knee.
- Muscular Imbalance– Runners who are excessively tight in the quadriceps muscles are prone to developing discomfort in their knees. Keeping up with a stretching regimen will help ease the symptoms.
- Older Age– Older runners tend to have some decrease in joint space due to wearing down of the tissues over the years. When the joint between the knee cap and knee wears down, there is more compression at the cartilage which can cause swelling and irritation of the local tissues. Every hear cracking, popping , or tearing when walking up and down stairs or with squats? Those are signs of cartilage wear called crepitus.
Runner’s Knee Treatment San Diego
Treatment for Runner’s knee involves 4 main approaches. The first is to address the injured tissue using Active Release Technique and Graston Technique. Active Release Technique for runner’s knee is effective at breaking down tight scar tissue around the knee. The second, using a running gait analysis to identify and correct common running form errors. Check out our full gait analysis for our patient with runner’s knee here: Runner’s Knee Case Study. The third is to modify the run training plan. Proper periodization is critical when coming back from injury. The goal is to modify certain factors (ex: terrain) that are known to irritate the knee. The fourth is to add strength training to the supporting muscle groups. This will provide more support, resist strain, and ultimately decrease chance of developing a running injury.
If you are experiencing pain in the front of the knee, you may be dealing with runner’s knee. It is important that you get the knee evaluated to get a proper diagnosis. This will help develop a correct treatment plan. Each person may benefit from slightly different approaches. The exercises and training modifications given to each patient are unique to the individual.
Our office is located in Mission Valley, San Diego near Normal Heights, La Mesa, Hill Crest, Point loma, Bay Park, Clairemont, Pacific Beach, and Bird Rock. Schedule online with one of our sports chiropractors today. We will help you get back to running pain free!
Chiropractic Care for Headaches
/in Headaches, Tips/by adminChiropractic Care for Headaches | San Diego Chiropractic
Summary
- Chiropractors are trained to diagnose the type of headache you are experiencing
- They are trained in manual therapies designed to treat muscles and joints that are causing or worsening the headaches
- They will work with you to identify reasons to why the muscles and joints are causing headache symptoms
- If there is a need for a referral, chiropractors can make sure you are sent to the right physician
- Our chiropractic office for treating headaches is located near La Mesa, Mission Gorge, Kensington, Serra Mesa, Bay Park, and Clairemont Mesa
- The types of headaches we treat are migraines, tension headaches, cervicogenic headaches, posture related headaches, trigger point referral headaches
Does Chiropractic Care Help Headaches?
Does chiropractic care help headaches? Chiropractic care can help reduce and even fully eliminate headache symptoms. Many headaches are due to muscle imbalances, and/or joint injury to the upper back, neck, and head region.
What Are Common Causes of Headaches?
Headaches are often experienced after trauma to the head and neck. They can also begin the develop over time as a result of poor posture or repetitive strain (same movements during sport, sitting at a desk 40 hours a week). As repetitive stress continues, the muscles and joints become irritated and start referring pain to the head region.
Pain referral patterns of muscles?
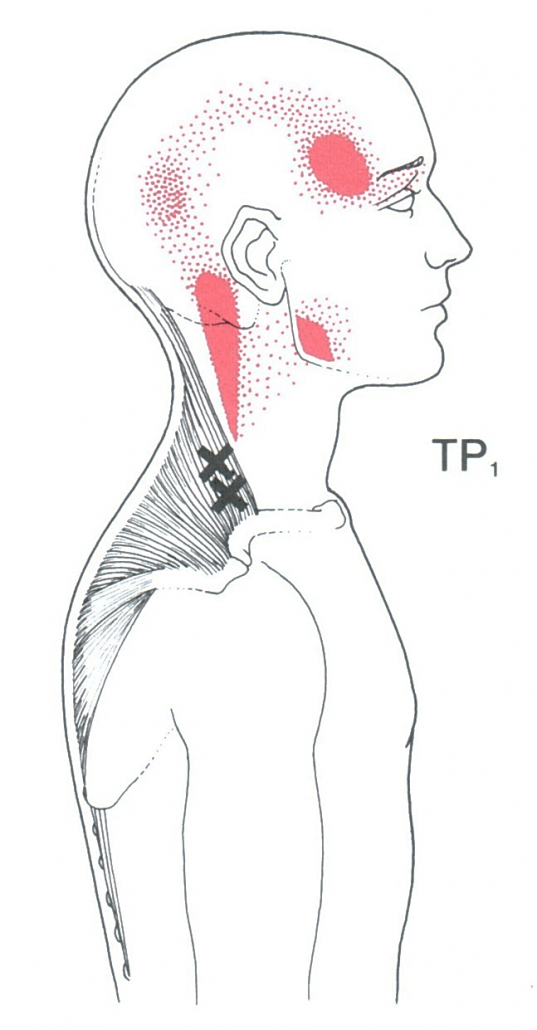
Upper Trapezius Trigger Point Referral
Acutely or chronically strained muscles can develop trigger points. Trigger points are hyper irritable fibers within a muscle unit that can cause local and referred pain. An active trigger point, actively causes pain. Example: pain in the muscles at the base of the skull with headache symptoms at eyeball area.
In this example, the muscle itself is sore and painful and is referring pain to the eyeball/forehead area. Another example is the upper trapezius muscle which connects the top of the shoulder to the neck. When that muscle develops a trigger point (often due to postural strain), headache symptoms can begin from the neck area up the side of the head, around the ear and to the temples. It looks like a question mark and headache symptoms can be felt anywhere along that path.
Ever tried rubbing your temples to get your headache to go away? Didn’t work? Try addressing the upper trapezius muscle which refers pain to the temples!
Pain Referral Patterns of the Joints
An inflamed and painful joint in the neck may also refer pain to various points of the neck, upper back, and head. Joints are normally injured through whiplash type injuries or quick movements without proper stabilization. Degenerative joints can also be a source of headache symptoms. As the joints wear down from past trauma and age, the degenerative joints compress the local tissues which then can refer pain.
There are plenty of referral patterns that result in headache symptoms. A chiropractor will evaluate the muscles and joints of the neck, shoulder, and upper back to identify the likely culprits. A proper referral will be made if the presenting symptoms are found to be outside of the musculoskeletal system.
Chiropractic Care for Common Headache Symptoms
In our San Diego based chiropractic office, we use a handful of therapies to treat common headache symptoms. Chiropractic adjustments or joint mobilization to the neck and upper back help restore motion to stiff, achy joints and relax local muscle tissues. Active Release Technique, and Graston Technique break down trigger points and tight muscles to eliminate muscular causes of headaches. Home exercises are then given to help combat headache symptoms and decrease the likelihood of the headaches returning.
Here is an example of how we treat a patient with neck and headache symptoms.
Why do the joints and muscles keep causing pain after treatment?
Many chiropractors, physical therapists, and other physical rehabilitation specialists claim they treat the “root cause” of your conditions. Many will treat the muscles and joints that cause the headaches as the “root cause”. Yes, that is treating what is causing the symptoms, but what is causing those muscles and joints to become irritated? Proper chiropractic care for headaches will also look at the entire picture. Here are a few likely causes for recurring headaches:
- Poor Posture
- Poor movement mechanics
- Diet
- Hydration
- Stress
- Sleep
Working working those categories, starting the most likely first, will identify the true cause of the headaches and eliminate them from returning!
Get Your Headaches Treated Today!
Our San Diego chiropractic team is trained to evaluate and treat your headaches. We are confident our chiropractic care for headaches will help reduce and even eliminate the frequency, intensity, and duration of the headaches you are experiencing. We are conveniently located in Mission Valley, San Diego near Ocean Beach, Pacific Beach, Normal Heights, and Hillcrest! Call or schedule online today!
How to Perform an Effective Hip Flexor Stretch
/in Back Pain Prevention, Conditions, Sports Injury/by adminA Safe and Effective Hip Flexor Stretch
The main muscles that make up the “hip flexors” are the rectus femoris, iliacus, and psoas major. This muscle group can become overactive and tight resulting in a variety of musculoskeletal issues. Many people perform a hip flexor stretch as a routine, or to help with a specific condition: knee pain, hip pain, back pain. Unfortunately, we see many patients who are performing a hip flexor stretch incorrectly and are exacerbating their condition. Take back pain as an example. Tight hip flexors can cause abnormal posture through the low back resulting in joint compression and irritation. Many patients will then stretch the hip flexors aggressively to help alleviate the symptoms. However, in an effort to loosen up the hip flexors, patients are compromising their low back by compressing a twisting the joints. To stretch the hip flexors properly, there are a few cues that you want to pay close attention to. Take a look at the following video; we go through the proper set up and execution of a safe hip flexor stretch.
Now, if you search “Best hip flexor stretch” you will get thousands of results and some are going to look really cool, and effective. At our chiropractic office in Mission Valley, San Diego we strive for keeping the exercises simple, accessible, and effective. Many of the “cool” or “aggressive” hip flexor stretches often put patients into compromised positions for their condition. Try this version of the hip flexor stretch. If you are suffering from low back, knee, or hip pain, please schedule with us to get a full evaluation. We specialize in treating sports injuries and tight hip flexors are a common presentation we see in our athletes as well as our workforce patients. Our office, Peak Form Health Center, is conveniently located off Texas Street, in Mission Valley, San Diego.
Sciatica- Conservative Management San Diego
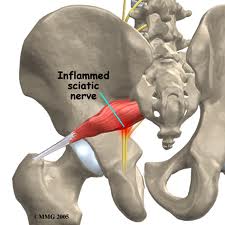
/in Conditions, Low Back Pain/by adminSciatica is a term that encompasses any condition that that can effect the sciatic nerve. Low back and hip injuries are the most common types of injuries that produce sciatica or sciatic symptoms. Less commonly, peripheral entrapment of the nerve around the hamstrings, and lower leg muscles cause sciatica symptoms in the back of the leg. Our San Diego chiropractor at Peak Form Health Center has treated countless conditions that cause sciatica symptoms.
What causes Sciatic Symptoms?
The sciatic nerve is made up of many different nerve roots from the low back and sacrum (tail bone). The nerve roots are extensions from the spinal cord that exit the spine to form peripheral nerves (ex: sciatic nerve is a peripheral nerve). If you have a back injury like a disc bulge, the disc bulge can press on the exiting nerve root which causes nerve irritation. Nerve irritation symptoms can cause numbness, tingling, hot/cold sensations, shooting pain, loss of sensation, and/or loss of function to the muscles that nerve innervates. Those same symptoms are what are described as “sciatica” but typically patients refer to sharp shooting pain as sciatica. Other conditions that can cause sciatica are:
- Low back injury- See our post on types of low back pain here: Different Types of Low Back Pain
- Disc bulge
- Disc herniation
- Piriformis syndrome– see our thorough blog post on piriformis syndrome here: Piriformis Syndrome: Overview and Causes Piriformis Syndrome Part II- Evaluation Piriformis Syndrome Part III- Treatment
- Degenerative Disc Disease
- Degenerative Joint Disease
- Foraminal stenosis of the lumbar spine (Bone Spurring)
- Central canal stenosis
- Sciatic nerve entrapment
- Spondylolisthesis
In rare but serious cases, sciatic symptoms may be due to: tumors, infection, tethered spinal cord, and other neurological conditions.
Conservative Management for Sciatica
First and foremost, a proper diagnosis is required to treat your symptoms effectively. Depending on what the cause is and how long it has been going on, usually a combination of manual therapy, specific exercise protocols, and home education can help resolve sciatica. Let’s take piriformis syndrome as an example. In piriformis syndrome, the piriformis muscles compresses the sciatic nerve. To treat this, targeted Active Release Techique and other myofascial release techniques often results in drastic improvement of symptoms. If however, the sciatica is due to a low back condition, manual therapy to the piriformis muscle will likely not result in significant relief of symptoms.
To reiterate the first point, it is important to see a sports chiropractor or sports medicine professional who will accurately diagnose what is causing the sciatica. Many times we see patients who have been dealing with sciatic symptoms for months and have been doing self treatments that are actually perpetuating their symptoms. Be very wary of a “do this one thing for your sciatica.” type blog post as it may be causing more harm than good.
Our San Diego based chiropractic group treats many different causes of sciatic symptoms. If there is ever concern of a more serious condition causing sciatica, or further investigation is required, we will make an appropriate referral to get the best care for you. Schedule today to get a thorough evaluation. Our office is conveniently located in Mission Valley, San Diego.
Big Toe Pain and Conservative Treatment
/in running injury, Sports Injury/by adminMany sports and activities of daily living require movement through the foot and big toe. When you are experiencing big toe pain, sports and certain activities can become quite difficult to perform. If your big toe pain is extreme, simple tasks such as standing, or walking can become very difficult. You may have heard of professional athletes missing months from their sport due to “turf toe” or other big toe conditions. The first thought (and I used to be guilty of this!) is, “It’s only your toe! Get out there and play!”. Well, if you are a 300 pound lineman in football and yue pressing through your big toe to try and stop an equally sized person, then there is tremendous load though a very small joint! When thinking of it from that perspective, it’s amazing that more athletes do not succumb to big toe pain and dysfunction.
Causes of Big Toe Pain
Acute Causes
Most commonly, a big toe joint can become sprained when it is bent backward or forward forcefully. This over stretches the joint and tendons in of the big toe. The following two acute conditions are commonly seen in our sports injury clinic:
Turf toe-Using a football lineman as an example again, when he is pressing forward and is met with equal or greater force by the opposing lineman, the big toe can get over stretched. Pain is generally felt on the bottom of the big toe and is difficult to walk due to the inability to push off.
Sand toe- A soccer player is playing barefoot on the beach and goes to kick the ball. She misreads the position of the ball on the sand and kicks the sand more than the ball. This forces the big toe joint downward, overstretching the top of the
joint and attached tendons.
Chronic Causes
We more commonly treat big toe pain due to chronic reasons. These conditions generally develop over time and are seen in middle aged and older patients (although these can affect younger populations in some cases). The following are common big toe conditions we treat:
- Hallux valgus
- Bunion deformity
- Sesamoiditis
- Functional hallux limitus
- Hallux rigidus
Structural issues
In many cases, especially associated with chronic conditions, foot structure may cause pain and dysfunction at the big toe. Most commonly, we see the following:
- Forefoot valgus
- Forefoot varus
- Plantarflexed first ray
- Subtle cavus foot
- Pes planus
- Pes cavus
Inflammatory conditions
Some patients deal with recurring inflammation of the big toe joint. There are a few inflammatory arthritides that can affect the big toe. The most common cause of big toe joint pain and inflammation is Gout. A referral to a rheumatologist is warranted if an inflammatory arthritis is suspected.
Evaluation
Our Sports Doctor of Chiropractic will evaluate the big toe, foot, ankle, lower leg, and possibly continue up the body into the lower back. Some conditions can be affected by muscle/joint dysfunction above where the pain is actually occuring.
Treatment
When it comes to big toe pain, Active Release Technique and Graston technique can help restore normal tissue function around the big toe. Chiropractic adjustments to the ankle, and midfoot can help with proper foot function to de-load the painful big toe joint. Exercises are also prescribed to strengthen/stretch the small muscles of the foot to improve big toe mobility. If there are structural issues present and a patient has recurring symptoms or does not improve with care, orthotics may be prescribed to accommodate the structural issue.
PEAK FORM NEWSLETTER SIGN UP
Our Office